Introduction
Reactive polycythemia (without presence of a chronic myeloproliferative neoplasm (MPN)) is commonly observed among patients with chronic pulmonary disease, whereas its significance in the context of COVID-19 is less well known. We aimed to investigate to what extent might polycythemia at the time of hospital admission affect outcomes of acutely ill COVID-19 patients.
Methods
We retrospectively evaluated a total of 5872 consecutive hospitalized COVID-19 patients treated in a tertiary referral center, UH Dubrava Zagreb, Croatia, in period 3/2020-6/2021. All patients were of white race and adults. All patients were tested positive for SARS-CoV-2 with either PCR or antigen test in the presence of compatible clinical symptoms. Patients with missing laboratory or clinical information or with prior or subsequently proven MPN were excluded from analysis. Hemoglobin threshold levels defined by the World health organization (WHO) criteria for diagnosis of anemia and the 2008 and 2016 WHO criteria for diagnosis of polycythemia vera (PV) were used to stratify patients into four subgroups (anemia, normal hemoglobin values, 2016 but not 2008 WHO polycythemia vera (PV), and 2008 WHO PV hemoglobin criteria fulfilling patients). Patients were evaluated in regard to baseline clinical characteristics, in hospital mortality, venous (VTE), arterial thrombosis and major bleeding.
Due to non-normal distribution, numerical variables were presented as median and interquartile range (IQR). The Kruskal Wallis ANOVA, the chi squared test and the logistic regression were used. P values <0.05 were considered statistically significant. All analyses were performed using the MedCalc statistical software version 22.007 (MedCalc Software Ltd, Ostend, Belgium).
Results
A total of 5872 COVID-19 patients were analyzed. There were 2575 (43.9%) female and 3297 (56.1%) male patients. Median age was 72 years, median Charlson comorbidity index was 4 points. A total of 4166 (70.9%) patients presented with severe and 897 (15.3%) with critical intensity of COVID-19 symptoms. Median hemoglobin level at the time of admission was 128 g/L, IQR (114-141). A total of 3082 (52.5%) patients presented with normal hemoglobin levels, 2607 (44.4%) with anemia, 158 (2.7%) fulfilled 2016 but not 2008 WHO PV hemoglobin criteria and 25 (0.4%) fulfilled 2008 WHO PV hemoglobin criteria.
Patients presenting with polycythemia in comparison to those with normal hemoglobin values were significantly older, were more likely to be of male sex, had higher Charlson comorbidity index, higher leukocytes, lower platelets, higher intensity of COVID-19 symptoms, required higher intensity of oxygen supplementation both at the admission and later during hospitalization (P<0.05 for all analyses).
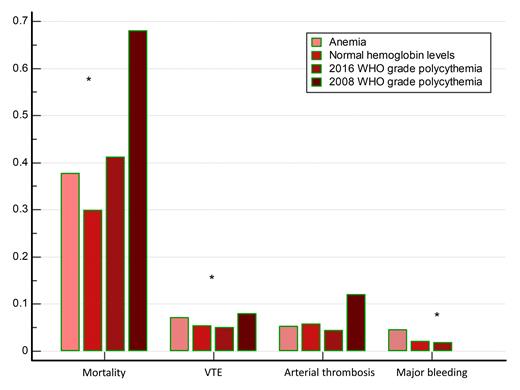
Figure 1 depicts the relationship of belonging to different hemoglobin categories with clinical outcomes. Patients presenting with anemia (OR 1.42, P<0.001), WHO 2016 grade (OR 1.63, P=0.003) and WHO 2008 grade polycythemia (OR 4.98, P<0.001) had increased risk of mortality in comparison to patients presenting with normal hemoglobin values. Anemia was associated with higher VTE (OR 1.34, P<0.006) and major bleeding risk (OR 2.27, P<0.001) in comparison to normal hemoglobin values, whereas no significant association of polycythemia with venous or arterial thrombotic or major bleeding risk was observed. Relationship of anemia, WHO 2016 and WHO 2008 grade polycythemia with increased mortality remained significant after adjusting analyses for age, sex, Charlson comorbidity index, COVID-19 severity and need for mechanical ventilation, all independently predicting inferior outcome (P<0.05 for all analyses).
Conclusion
Secondary polycythemia in non-MPN COVID-19 patients is associated with high mortality, increasing with higher degree of polycythemia, but does not seem to affect thrombotic or major bleeding risk in comparison to normal hemoglobin values. These observations might help in understanding risks associated with polycythemia and increased blood viscosity in the context of other respiratory diseases. These findings might also translate into the context of MPN and COVID-19, suggesting that blood cells other than erythrocytes might play a more important role regarding thrombotic risk. Future studies are warranted.
Disclosures
Krecak:Janssen: Honoraria.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal